Keep It Moving – Spinal Artificial Disc Replacement
What is arthroplasty?
As the long-term effects of aging, injury or arthritis become limiting, the Holy Grail of pain free mobility has proven to be joint replacement (arthroplasty). For millions of people around the world, the benefits of hip, knee and a variety of other joint implantation are well known. However, it has been a challenge for spine surgeons and researchers to develop a similar fix for patients suffering from intractable neck and back pain; therefore, artificial disc replacement (ADR) has lagged behind. The good news is that new, innovative developments in disc arthroplasty are beginning to change the landscape.
How does the spine work?
The spinal column is a particularly complex structure, protecting the spinal cord and the nerves that innervate organs and muscles and send sensory information back to the brain; all this, while supporting the upright body and allowing movement throughout the neck and back. The components of the spinal column consist of vertebral bodies and intervertebral discs positioned between the vertebrae. The intervertebral disc is not a true joint, such as the hip or knee, but is made up of a dense fibrous ring (annulus fibrosis) filled with compressible gel-like tissue (nucleus pulposus). These two elements of the disc allow the vertebral bodies to move with six degrees of freedom and provide compressibility while helping maintain the structural integrity of spine.
What is the problem with the disc?
Once the disc starts to fail — for example, developing annular tears, nucleus dehydration and collapse — for many, it brings with it severe neck, back and/or extremity pain. Unfortunately, although regenerative treatment modalities may hold promise in the future, we are not yet able to reverse the effects of intervertebral disc failure. Therefore, once all conservative and interventional pain management methods have been exhausted, fusion of the vertebrae across the disc space has been the standard treatment option.
How does the artificial disc work?
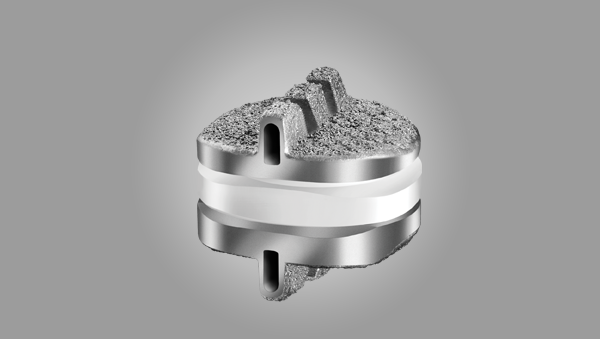
Several lumbar and cervical artificial disc replacement devices have been cleared for use in the USA by the FDA and are being implanted by spine surgeons with excellent short- and long-term results. These devices are innovative constructs which facilitate movement through the disc space, although not to the same extent as the healthy intervertebral disc itself. The majority have three distinct moving parts –- two end plates that interface with the vertebral bodies and a central core that promotes movement and, in a couple of instances, compressibility. While most are approved for single level disc degeneration surgery, FDA authorization for two level implantation in the cervical spine has been granted for some devices, as well.
How do I know if it’s right for me?
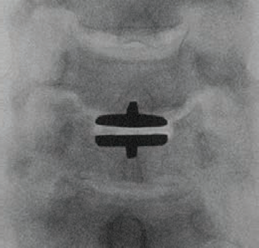
Follow up studies on patients indicate excellent results from cervical and lumbar disc arthroplasty, when compared to fusion. Unlike with instrumented fusion surgeries, requiring screws and rods, there appears to be a lower risk of breakdown of the disc space above or below the operative level. Also, with ADR there is no concern about the healing of bone fusions, which may be a problem in high risk patients, such as smokers. Most operations are performed in an out-patient setting and recovery from ADR surgery appears to be easier, with patients returning to regular activities of daily living in 12-weeks. However, some may not qualify for ADR, for reasons including severe disc space collapse that would limit the ability to implant the device, more than two levels of involvement, spinal instability or deformity and the presence of fractures, tumor or infection.
What do I do next?
MBSP surgeons are experts at artificial disc replacement and we have participated in multi-center trials that have helped to bring some of these devices to market. With each new patient, we conduct a thorough clinical evaluation, including review of up-to-date imaging studies (X-ray, CT or MRI). Once the clinical evaluation is complete, a decision is reached about the most appropriate course of action for each, specific patient. As always, we strive to address these problems with the least invasive and most appropriate treatment option available to the individual.